When Your Brain Stops Working Right: Is It Menopause or Dementia?
October 27, 2025
What estrogen does to your brain
You're forgetting names of people you've known for years. Walking into rooms with zero idea why you're there. Losing words mid-sentence. Staring at things you wrote yesterday and not recognizing them.
If this is happening in your 40s or 50s, you're probably terrified it's early-onset dementia. It's probably not. Let me explain what's actually going on with your brain during perimenopause.
Everyone thinks estrogen just handles periods and reproduction. Wrong. Estrogen is premium maintenance service for your brain.
It keeps neurons healthy and helps them communicate with each other. It supports production of serotonin, dopamine, and acetylcholine - brain chemicals controlling mood, attention, and memory. It enhances blood flow to your brain. It protects against oxidative stress and inflammation. It helps you form new memories and retrieve old ones. It maintains myelin - the insulation around nerve fibers. It supports neuroplasticity - your brain's ability to adapt and change.
When estrogen fluctuates wildly during perimenopause - sky high one week, crashed the next - your brain feels every single swing.
When it drops permanently in menopause, your brain has to figure out how to function without this critical support system.
That's what you're feeling. Not dementia. Estrogen withdrawal affecting your cognitive function.
What Are the Cognitive Symptoms of Perimenopause?
- Memory becomes completely unreliable. You can't remember what someone told you five minutes ago. You know you know something but can't retrieve it when you need it. You forget entire conversations that apparently happened. You misplace everything because you don't remember putting it down.
- Processing speed slows way down.Everything feels like it's moving through molasses. Multitasking becomes impossible when you used to juggle ten things easily. Your brain feels sluggish. You need extra time to formulate responses that used to come instantly.
- Words disappear mid-sentence. You're talking and suddenly the word just vanishes. Common vocabulary becomes elusive. You end up describing objects instead of naming them because the actual name won't come to you.
- Concentration is completely shot. You start tasks and your mind wanders constantly. You're distracted by everything. Complex projects feel overwhelming when they used to be straightforward. You read the same paragraph five times and it still doesn't stick.
- Executive function struggles. Planning and organizing become confusing. Simple decisions feel impossible. Prioritizing tasks is hard. Adapting to changes or new situations is harder than it used to be.
This is hormonal brain fog during perimenopause. It's incredibly common. And it's absolutely terrifying when nobody explains what's happening to your brain.
How Is Menopause Brain Fog Different From Dementia?
Doctors hear these cognitive complaints and immediately think cognitive decline. But hormonal brain fog and actual dementia are completely different:
Hormonal brain fog:
- Appears suddenly around perimenopause
- Fluctuates - worse some weeks, better others
- Mainly affects word retrieval and processing speed
- You're acutely aware something's wrong
- Usually comes with other menopausal symptoms like hot flashes or night sweats
- **It's reversible**
Actual dementia:
- Develops gradually over months to years
- Consistently worsens without fluctuation
- Affects recognition, not just retrieval - you don't recognize familiar people or places
- You're often unaware of the deficits
- Usually appears after age 65
- **It's not reversible
The patterns are different. The timing is different. The reversibility is completely different.
Why Don't Doctors Connect Brain Fog to Hormones?
Most physicians don't ask about menstrual cycles when cognitive symptoms appear. They hear "memory problems" in a woman over 40 and think neurological disease, not hormones.
They order expensive dementia workups - brain MRI, extensive cognitive testing, sometimes PET scans - before considering that estrogen fluctuations might be causing these symptoms.
They prescribe antidepressants for brain fog without investigating whether hormones are the actual issue.
They dismiss symptoms as "normal aging" or "you're just stressed" without recognizing the specific pattern of menopausal cognitive changes.
They weren't trained in menopause medicine. Only one in five OB-GYN residents gets formal menopause training. If your gynecologist didn't learn this, your primary care doctor almost certainly didn't either.
How Poor Sleep Makes Brain Fog Worse
Poor sleep quality during menopause directly impacts cognition in ways that look exactly like cognitive decline.
Your brain clears metabolic waste during deep sleep. Without adequate deep sleep, waste products accumulate. Memory consolidation happens during sleep - your brain transfers information to long-term storage. Disrupted sleep from night sweats prevents this transfer. Chronic sleep deprivation mimics cognitive decline - attention problems, memory issues, slowed processing, difficulty concentrating.
If night sweats or insomnia are disrupting your sleep, fixing that hormonal issue often dramatically improves cognitive function. The brain fog wasn't dementia. It was sleep deprivation caused by hormonal symptoms.
I've seen this pattern repeatedly. Women convinced they have early dementia, terrified they're losing their minds. We address their sleep disruption through hormone optimization, and suddenly their "cognitive decline" reverses.
What Actually Helps Menopausal Brain Fog
Hormone optimization through bioidentical hormone therapy.
For many women, appropriately restoring estrogen improves memory formation and retrieval, enhances processing speed, reduces brain fog, and restores verbal fluency. Research shows women starting hormone therapy within 10 years of menopause may have cognitive benefits and potentially reduced dementia risk later in life.
Not everyone's a candidate for hormone therapy. But if cognitive symptoms started during your hormonal transition, discuss this with a menopause specialist.
TMS (Transcranial Magnetic Stimulation).
TMS enhances neuroplasticity, improves cognitive processing, and supports focus and concentration. It has no systemic side effects. For women with significant cognitive symptoms during menopause, TMS can provide substantial support while the brain adapts to hormonal changes.
Fix sleep quality first.
Seven to nine hours consistently. Address the root causes of night sweats and insomnia - these hormonal symptoms need treatment, not just sleep hygiene tips. Consider sleep studies if disruption continues despite good habits. But recognize that perfect sleep hygiene won't overcome hormonal sleep disruption.
Regular exercise for brain health.
Movement increases BDNF (Brain-Derived Neurotrophic Factor) which supports neuron growth and survival. It enhances neuroplasticity. It improves blood flow to your brain. It reduces inflammation. Both cardiovascular exercise and resistance training help cognitive function. Consistency matters more than intensity.
Brain-supporting nutrition.
Omega-3 fatty acids support neuron health. Adequate protein provides amino acids for neurotransmitter production. B vitamins, especially B12 and folate, are critical for brain function. Vitamin D - most midlife women are deficient. Antioxidants from colorful vegetables protect brain cells. Limit added sugars - high blood sugar damages brain cells over time.
Stress management for cognitive protection.
Critical for protecting your hippocampus (memory center) from cortisol damage. Find what actually works for you to lower stress response. Nature. Yoga. Meditation. Time with friends. Therapy. Setting boundaries at work and home.
Start Addressing Brain Fog Today
- Track your cognitive symptoms in relation to your menstrual cycle if you still have one. Look for patterns.
- Prioritize sleep as non-negotiable. Make it a top health priority.
- Add movement to your routine. Even walking helps brain function.
- Request appropriate testing - hormones and nutrient levels before jumping to dementia workup.
- Explore hormone therapy with knowledgeable menopause specialists who understand cognitive symptoms.
- Consider TMS if cognitive symptoms are significantly affecting your work or daily life.
- Your brain isn't deteriorating into dementia. It's responding to dramatic hormonal changes without adequate support.
Cognitive symptoms during perimenopause and menopause are extremely common, highly treatable, and often completely reversible with comprehensive care that addresses the hormonal foundation of brain health.
Concerned about memory loss and brain fog during menopause? Check out the Midlife Edit

Meet the Author
You might also enjoy:

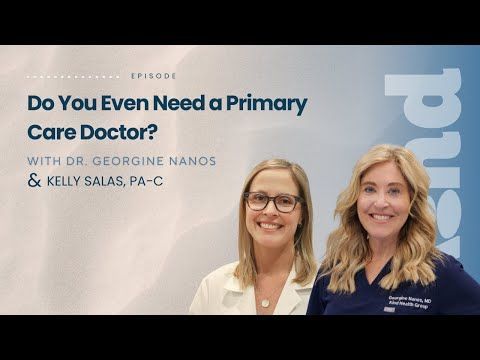
Longevity medicine is a trillion-dollar industry—but what actually works? Dr. Georgine Nanos, board-certified physician with 20+ years of family medicine experience, separates wellness theater from real science in this honest conversation about supplements, detoxes, brain health, heart disease, GLP-1s, and the fundamentals that truly impact how long and how well you live.
In this episode:
⏱️ 0:00 - Introduction
⏱️ 3:17 - Why the wellness industry is exploding (and who's profiting)
⏱️ 5:30 - What actually works: The unsexy fundamentals
⏱️ 7:01 - "Wellness theater" explained—the illusion of health
⏱️ 8:47 - The truth about detoxes and cleanses (spoiler: your liver already does this)
⏱️ 11:57 - Supplement dangers: Why "natural" doesn't mean safe
⏱️ 13:58 - PSA: Tell your doctor what supplements you're taking
⏱️ 15:53 - Brain health and longevity: The stress-aging connection
⏱️ 19:49 - Heart disease: The #1 killer no one talks about
⏱️ 22:17 - GLP-1 medications: Why they're revolutionary
⏱️ 27:18 - VO2 max and Zone 2 training: Simple cardio that extends life
⏱️ 31:19 - Why patients distrust doctors (and it's not the doctors' fault)
⏱️ 35:55 - Red flags: Spotting fake "experts" online
⏱️ 38:55 - Where to start in 2026 without burning out
📍 Kind Health Group is a San Diego-based integrative primary care practice offering comprehensive wellness programs, advanced cardiac testing, brain health services
🔗 CONNECT WITH US:
Website: kindhealthgroup.com
Instagram: @kindhealthgroup
Gallery Test (cancer screening)
Prenuvo MRI
InBody scans
Zone 2 training research
GLP-1 medications (Ozempic, Wegovy, etc.)
💬 If this episode helped you feel more grounded about your health, share it with someone who needs that reminder.
This is The Kind Revolution Podcast—subscribe for more conversations about brain health, longevity, and transforming how we think about healthcare.