You Don't Need More Specialists. You Need Someone Who Sees the Whole Picture.
November 3, 2025
Why this system is designed to fail midlife women.

In this blog:
- Why the specialist shuffle is making you sicker, not better
- The hidden costs nobody talks about
- What actually happens when your healthcare team coordinates
- Real solutions that address root causes instead of playing symptom whack-a-mole
Tuesday morning, 9:30 AM. Jennifer sits in her endocrinologist's waiting room, filling out the same medical history form she's filled out fourteen times in the past six months. Different doctor, same questions, same frustration.
Her phone calendar shows the rest of her week: rheumatologist Thursday, dermatologist Friday, sleep specialist next Tuesday. Each appointment requires driving across town, finding parking, sitting in a waiting room that smells like industrial cleaner and despair, and explaining her entire medical history to someone who has twelve minutes to "fix" one isolated symptom.
Nobody's looking at the big picture. Nobody's connecting the dots between her aching joints, her exhausted brain, her terrible sleep, and the twenty pounds that appeared overnight around her middle.
Look, I get it. This is how medicine works now. You go to your primary care doctor, they refer you out to specialists, those specialists order tests and prescribe treatments, and somehow you're supposed to coordinate all of this while also, you know, living your actual life.
But here's what nobody tells you: this system wasn't designed for women going through perimenopause and menopause. It was designed to treat acute problems in isolated organ systems. Heart attack? Cardiologist. Broken bone? Orthopedist. Skin cancer? Dermatologist.
The system falls apart completely when your estrogen drops and suddenly everything is connected to everything else.
Let me walk you through what actually happens.
Your joints hurt. Primary care says that's probably arthritis, go see rheumatology. Three weeks to get that appointment, another round of blood tests, some anti-inflammatory medication that tears up your stomach.
Your brain's not working right. That doctor says maybe depression, go see psychiatry. More waiting, a prescription for an SSRI that makes you gain weight and kills your sex drive.
You can't sleep. Sleep specialist orders a study, tells you that you have some mild apnea, suggests a CPAP machine you'll never actually use.
Your skin looks like hell. Dermatologist prescribes expensive creams that don't work because the problem is hormonal, not topical.
And the whole time, nobody's asking the most obvious question: what if all of this is connected? What if Jennifer's joints hurt because dropping estrogen is causing inflammation? What if her brain fog is because she's not sleeping, and she's not sleeping because her hormones are wrecked, and her hormones are wrecked because nobody's actually managing her menopause?
But that's not how the system works. The system rewards volume. Insurance pays for fifteen-minute visits focused on one chief complaint. Electronic medical records don't talk to each other. Nobody has time to read through your stack of records from five other doctors.
So you end up being your own case manager, coordinator, and medical detective. Except you don't have a medical degree, you're exhausted, and honestly, you shouldn't have to do this.
The Real Cost Nobody Calculates
Jennifer tallied it up last month. She'd spent $847 on co-pays. Taken nine half-days off work. Driven 143 miles to various medical offices. Repeated her medical history seventeen times. Filled twelve different prescriptions.
Her symptoms hadn't improved.
That's just the money and time. The actual cost is so much bigger.
It's the mental load of tracking everything yourself. Remembering which doctor prescribed what. Noticing that two of your specialists prescribed medications that interact. Trying to explain to your gynecologist what your rheumatologist said about your inflammation markers.
It's the emotional exhaustion of telling your story over and over to people who are already half-listening because they're behind schedule. Of being reduced to symptoms instead of treated as a whole person. Of feeling like you're the problem because nothing's getting better.
It's the physical toll of having multiple conditions treated in isolation when they're actually all manifestations of the same hormonal chaos.
Jennifer told me last month that she felt like she was losing her mind. "I'm doing everything they tell me to do. I take all the medications. I go to all the appointments. But I feel worse than I did a year ago. What am I doing wrong?"
Nothing. The system is doing everything wrong.
Here's what happened when Jennifer came to Kind Health Group.
First appointment: ninety minutes. Not because we're inefficient, but because we actually needed to understand her complete picture. Her symptoms, yes. But also her life. Her stress levels. Her sleep patterns. Her exercise routine. Her diet. Her relationships. Her goals.
We did comprehensive hormone testing. Not just TSH and maybe FSH if you're lucky, but everything - estrogen, progesterone, testosterone, DHEA, cortisol throughout the day. Complete metabolic panel. Inflammatory markers. Nutrient levels.
And then we actually looked at how everything connected.
Her joint pain? Inflammatory response to dropping estrogen, plus vitamin D deficiency, plus poor sleep quality creating more inflammation. Her brain fog? Combination of sleep deprivation, hormone changes affecting neurotransmitter production, and probably some insulin resistance. Her weight gain? Metabolic changes from hormone loss, plus cortisol dysregulation from chronic stress and poor sleep, plus insulin resistance making everything worse.
None of this was separate. It was all the same problem showing up in different ways.
Jennifer's plan included bioidentical hormone replacement - estrogen and progesterone dosed appropriately for her specific situation. Vitamin D supplementation at therapeutic levels. Specific nutrition changes to support insulin sensitivity. A sleep protocol that didn't involve sleep medication.
We added TMS for her brain health and mood support because when you're this exhausted and overwhelmed, your brain needs some help getting back online. Exosella for her pelvic floor weakness that nobody had connected to her back pain and core instability.
Three months in, Jennifer came back for follow-up. Her joint pain was 80% better. Her brain fog was gone. She'd lost eight pounds without trying because her metabolism was working again. She was sleeping through the night.
"Nobody ever told me this was all connected," she said. "I thought I was just falling apart in seven different ways."
That's the thing. You're not falling apart in seven different ways. Your body is responding to a major hormonal transition, and that transition affects multiple systems simultaneously. Treating each symptom separately doesn't work because you're not addressing the root cause.
If you're done with the specialist shuffle, here's what comprehensive midlife care should include.
Real hormone management. Not just "your labs are normal" when you feel terrible, but optimization of your hormone levels to support how you actually want to live. Understanding that "normal" ranges are based on averages of sick people, not optimal levels for a woman who wants to feel like herself.
Metabolic support. Because dropping estrogen tanks your metabolism, and you can't reverse that with willpower and salads. You need actual intervention - sometimes medication, always nutrition and exercise prescription based on your specific physiology.
Brain health optimization. Your brain is an endocrine organ. When hormones change, brain function changes. TMS can help optimize neural pathways. Proper sleep protocols. Stress management that actually works.
Aesthetic treatments that work with your changing physiology. Your skin is changing because of hormones, not because you need better moisturizer. Treating aesthetic concerns means understanding the hormonal foundation.
Mental health integration. Because sometimes what looks like depression or anxiety is actually hormonal chaos. And sometimes hormonal chaos creates real mood disorders that need treatment. But you need someone who can tell the difference.
All of this coordinated by a team that actually talks to each other about you.
The Kind Health Group Approach
Look, I'm obviously biased here. But I'll tell you exactly how we do this.
Your first visit is comprehensive. We're looking at everything - complete hormone panel, metabolic markers, inflammatory markers, nutrient status. Full history of your symptoms and how they're affecting your actual life. Discussion of your goals beyond just "feeling better."
Then we build a coordinated treatment plan. Hormone optimization as the foundation because you can't fix anything else if your hormones are wrecked. Metabolic support through nutrition and sometimes medication. Sleep protocols. Brain health through TMS when beneficial. Aesthetic treatments when desired, timed appropriately with other interventions.
Regular follow-up where we adjust based on your response. Not just "how are your symptoms" but "how's your life." Because the goal isn't just symptom management. It's optimal function.
And here's the key part: everyone on your team knows everything about your care. When we add a treatment, we're considering how it fits with everything else you're doing. When something's not working, we're looking at the whole picture to figure out why.
If you're stuck in the specialist shuffle, start here.
Document everything. List all your symptoms, even the ones that seem unrelated. Track when they're worse or better. Note any patterns. Bring this to your next appointment.
Request coordination. Tell your doctors you want them to communicate with each other. Ask them to send notes to your other providers. Keep your own records because the system won't do this automatically.
Look for comprehensive programs specifically designed for midlife women. Not just a menopause clinic, but actual coordinated care addressing hormone optimization, metabolic health, brain health, and aesthetic concerns if relevant.
Ask about provider qualifications. Do they have training in menopause medicine? Do they understand hormone optimization beyond "throw some estrogen at it"? Will they actually coordinate with other specialists?
Trust your gut. If a doctor dismisses your symptoms as "just aging" or won't discuss hormone therapy, find someone else. If nobody's looking at how your symptoms connect, you're in the wrong place.
You don't need seven specialists who don't talk to each other. You need one team that understands midlife hormonal changes
affect everything and treats you as a complete human being, not a collection of isolated symptoms.
Jennifer told me last week she wishes she'd found coordinated care three years ago. "I thought I was just supposed to deal with getting older. I didn't know this was fixable."
It is fixable. But not through the standard medical system designed for acute care and isolated organ systems. You need someone actually trained to manage the comprehensive, interconnected changes of midlife.
Your body isn't falling apart. It's going through a major transition that affects multiple systems simultaneously. You need care that understands that. Learn more about the Kind Midlife Edit.

Meet the Author
You might also enjoy:

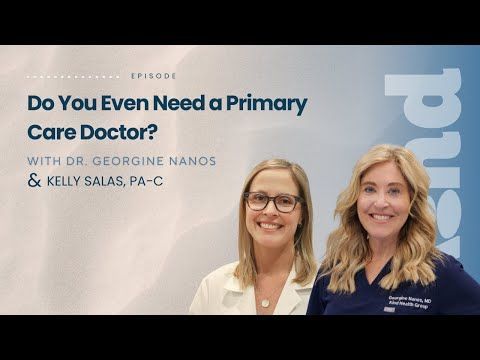
Longevity medicine is a trillion-dollar industry—but what actually works? Dr. Georgine Nanos, board-certified physician with 20+ years of family medicine experience, separates wellness theater from real science in this honest conversation about supplements, detoxes, brain health, heart disease, GLP-1s, and the fundamentals that truly impact how long and how well you live.
In this episode:
⏱️ 0:00 - Introduction
⏱️ 3:17 - Why the wellness industry is exploding (and who's profiting)
⏱️ 5:30 - What actually works: The unsexy fundamentals
⏱️ 7:01 - "Wellness theater" explained—the illusion of health
⏱️ 8:47 - The truth about detoxes and cleanses (spoiler: your liver already does this)
⏱️ 11:57 - Supplement dangers: Why "natural" doesn't mean safe
⏱️ 13:58 - PSA: Tell your doctor what supplements you're taking
⏱️ 15:53 - Brain health and longevity: The stress-aging connection
⏱️ 19:49 - Heart disease: The #1 killer no one talks about
⏱️ 22:17 - GLP-1 medications: Why they're revolutionary
⏱️ 27:18 - VO2 max and Zone 2 training: Simple cardio that extends life
⏱️ 31:19 - Why patients distrust doctors (and it's not the doctors' fault)
⏱️ 35:55 - Red flags: Spotting fake "experts" online
⏱️ 38:55 - Where to start in 2026 without burning out
📍 Kind Health Group is a San Diego-based integrative primary care practice offering comprehensive wellness programs, advanced cardiac testing, brain health services
🔗 CONNECT WITH US:
Website: kindhealthgroup.com
Instagram: @kindhealthgroup
Gallery Test (cancer screening)
Prenuvo MRI
InBody scans
Zone 2 training research
GLP-1 medications (Ozempic, Wegovy, etc.)
💬 If this episode helped you feel more grounded about your health, share it with someone who needs that reminder.
This is The Kind Revolution Podcast—subscribe for more conversations about brain health, longevity, and transforming how we think about healthcare.