Stop Playing Medical Whack-a-Mole: Why Your Symptoms Are Connected
October 20, 2025

In this blog, you will find:
• Why bouncing between specialists for scattered symptoms doesn't work
• How one hormone affects your joints, brain, metabolism, sleep, and skin at the same time
• The biological domino effect that makes symptoms worse when treated separately
• What comprehensive midlife care actually looks like
• Steps you can take right now to address root causes instead of symptoms
___________________
She's 47. Used to run marathons. Now she can't remember where she parked.
"I'm basically a full-time project manager for my own body," she said. "And none of these people talk to each other."
This is what passes for women's healthcare right now. It's completely backwards.
Here's what actually happened: Around 45, her periods got weird. Six months later, her knees started hurting during runs. Then she couldn't remember client names. Then fifteen pounds appeared out of nowhere. Then sleep vanished entirely.
Five problems. Five specialists. Zero connection between them.
The rheumatologist ordered MRIs and prescribed anti-inflammatories. The psychiatrist suggested antidepressants for "cognitive symptoms." The endocrinologist started metformin. The sleep doctor gave her Ambien. The dermatologist handed her retinol.
Not one of them asked about her cycle.
Estrogen isn't just about periods. It runs your entire body.
Your joints need it for cartilage and lubrication. When it drops during perimenopause, inflammation goes up. That's why you suddenly have pain even though your imaging looks fine.
Your brain uses it to protect neurons and help neurotransmitters work. When it crashes, memory goes. Concentration disappears. This gets called depression when it's actually estrogen withdrawal.
Your metabolism needs it for insulin sensitivity and fat distribution. Without it, cells stop responding to insulin, metabolism slows, and fat goes to your belly.
Your sleep depends on it for temperature control. When it's erratic, you're up all night. Exhaustion makes everything else worse.
Your skin needs it for collagen. When it drops, you age faster.
One hormone. All of it connected.
But you get sent to the joint person who only knows joints. The brain person who only knows brains. Nobody's asking why this all started at once.
You can't sleep from night sweats. Exhaustion spikes stress hormones. Stress increases inflammation throughout your body. Inflammation worsens joint pain. Pain stops exercise. Less movement means muscle loss. Less muscle slows metabolism. Slower metabolism means weight gain. Weight gain increases inflammation. More inflammation disrupts sleep.
Each specialist treats their piece. But the whole system keeps breaking because nobody's looking at why.
I see this pattern every single day—women bouncing between specialists for months or years, getting diagnosed with five different conditions, when the real issue is their hormones changed and nobody connected the dots.
Another patient came to me on five medications from four different specialists. Joint pain, brain fog, weight gain, insomnia, mood swings.
We addressed her hormones through bioidentical hormone replacement therapy. Eight weeks later, she'd stopped three medications.
Joint pain improved so she could move again. Better sleep normalized stress hormones. Lower stress meant less inflammation. Less inflammation meant her joints hurt less. More movement improved metabolism. Better metabolism helped mood and energy.
Not magic. Just addressing what was actually causing everything instead of playing symptom whack-a-mole.
Track everything together. When sleep is bad, does brain fog get worse? When stress is high, do joints hurt more? Bring the complete picture to appointments instead of isolated complaints.
Get comprehensive hormone testing. Full hormone panels, not just FSH to confirm menopause. Complete thyroid panel, not just TSH. Inflammation markers like hs-CRP. Fasting insulin to check metabolic health. Actual data about what's happening.
Ask if symptoms might be connected.
When a doctor wants to treat one symptom, ask if hormonal changes could be involved. Ask if your other symptoms might be related. Push back on being split into separate problems requiring separate specialists.
Find a menopause specialist.
Not every doctor who treats women understands perimenopause and menopause. Look for NAMS certification (North American Menopause Society). Ask about their experience with hormone optimization. Experience with midlife women matters.
Consider hormone optimization.
If multiple symptoms started during perimenopause, talk to someone knowledgeable about whether bioidentical hormone therapy might address several issues at once.
Your scattered symptoms aren't random separate problems needing different specialists.
They're connected responses to hormonal changes during perimenopause that deserve coordinated treatment.
When you address the hormonal foundation, everything built on it can improve together. Joints. Brain. Metabolism. Sleep. All of it.
Stop the specialist shuffle. Treat your health as the connected system it is.
Ready to stop playing medical whack-a-mole? Learn about The Kind Mid-Life Edit
where we address the root causes of perimenopause symptoms instead of just managing them separately.

Meet the Author
You might also enjoy:

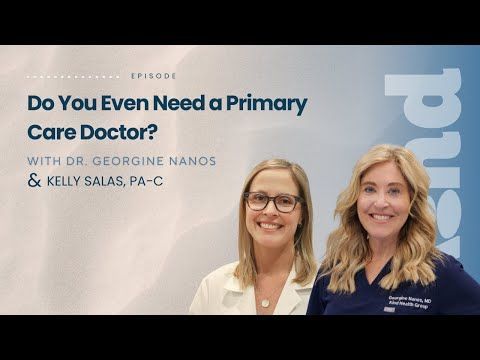
Longevity medicine is a trillion-dollar industry—but what actually works? Dr. Georgine Nanos, board-certified physician with 20+ years of family medicine experience, separates wellness theater from real science in this honest conversation about supplements, detoxes, brain health, heart disease, GLP-1s, and the fundamentals that truly impact how long and how well you live.
In this episode:
⏱️ 0:00 - Introduction
⏱️ 3:17 - Why the wellness industry is exploding (and who's profiting)
⏱️ 5:30 - What actually works: The unsexy fundamentals
⏱️ 7:01 - "Wellness theater" explained—the illusion of health
⏱️ 8:47 - The truth about detoxes and cleanses (spoiler: your liver already does this)
⏱️ 11:57 - Supplement dangers: Why "natural" doesn't mean safe
⏱️ 13:58 - PSA: Tell your doctor what supplements you're taking
⏱️ 15:53 - Brain health and longevity: The stress-aging connection
⏱️ 19:49 - Heart disease: The #1 killer no one talks about
⏱️ 22:17 - GLP-1 medications: Why they're revolutionary
⏱️ 27:18 - VO2 max and Zone 2 training: Simple cardio that extends life
⏱️ 31:19 - Why patients distrust doctors (and it's not the doctors' fault)
⏱️ 35:55 - Red flags: Spotting fake "experts" online
⏱️ 38:55 - Where to start in 2026 without burning out
📍 Kind Health Group is a San Diego-based integrative primary care practice offering comprehensive wellness programs, advanced cardiac testing, brain health services
🔗 CONNECT WITH US:
Website: kindhealthgroup.com
Instagram: @kindhealthgroup
Gallery Test (cancer screening)
Prenuvo MRI
InBody scans
Zone 2 training research
GLP-1 medications (Ozempic, Wegovy, etc.)
💬 If this episode helped you feel more grounded about your health, share it with someone who needs that reminder.
This is The Kind Revolution Podcast—subscribe for more conversations about brain health, longevity, and transforming how we think about healthcare.